You can learn a lot about a person by their fingernails, especially when it comes to health. Anomalies such as changes in shape and color can indicate medical conditions such as psoriasis, heart disease, and even cancer. But keep in mind that brittle or discolored nails are not typically a cause for alarm since they can come from injuries, dampness, poor nutrition, or age.
Advertisement
“For the general population, nail health is most often an indicator of poor nutritional intake or poor digestion,” explains Dr. Sara Norris, a naturopathic doctor based in Los Angeles. “Brittle, weak, and peeling nails are the most common concerns I see in my practice and these symptoms are more often the result of a poor diet than of systemic disease.”
So don’t panic if your nails resemble these descriptions. But if the issue doesn’t resolve on its own or if it accompanies other symptoms (like fatigue, weakness, swelling, heart palpitations, weight loss, etc.) speak to a medical practitioner.
Beau’s lines

“Deep lines or grooves across your fingernails are known as Beau’s lines,” says Dr. Bhavini Shah of Lloyds Pharmacy Online Doctor. These lines appear when nail growth has briefly slowed or stopped. “This temporary disturbance of nail growth is usually caused by severe illness or infection. Some people developed Beau’s lines after they had COVID-19, for example.” In severe cases, the nail can stop growing long enough to form a full gap, which is medically known as onychomadesis. This can occur after major stresses like chemotherapy, injuries, and high fevers.
One of the most common causes of Beau’s lines is physical trauma to the nail or finger. A severe injury, such as slamming your finger in a door or hitting it with a hammer, can temporarily damage the nail matrix, leading to the formation of ridges. However, trauma is not the only cause. Severe illnesses, such as pneumonia, heart attack, or uncontrolled diabetes, can also result in the appearance of Beau’s lines. In these cases, the body prioritizes essential functions to fight the illness, temporarily halting or slowing non-essential processes like nail growth.
In addition to injuries and illnesses, environmental factors can sometimes contribute to the development of Beau’s lines. Prolonged exposure to harsh chemicals, repeated use of nail polish or acrylic nails, or frequent handwashing with abrasive soaps can stress the nail matrix and lead to these distinctive ridges. Similarly, nutritional deficiencies, such as a lack of zinc, calcium, or biotin, can also play a role in disrupting normal nail growth.
Beau’s lines can also indicate chronic medical conditions. For example, diseases that cause inflammation throughout the body, such as lupus or rheumatoid arthritis, can sometimes leave their mark on the nails. Additionally, certain chemotherapy drugs and other medications may cause Beau’s lines as a side effect.
One intriguing aspect of Beau’s lines is that they can provide a timeline of the health event that caused them. Nails grow at an average rate of about 3 millimeters per month, so the position of the ridge on the nail plate can give doctors an estimate of when the disruption occurred. If the ridges are close to the cuticle, the event was recent. If they are closer to the tip of the nail, the event happened several months ago.
Diagnosing the cause of Beau’s lines often requires a careful review of a person’s medical history, along with a physical examination. In some cases, additional tests may be necessary to rule out specific conditions. While Beau’s lines themselves are not harmful, they are almost always a symptom of an underlying issue that needs to be addressed.
Treatment for Beau’s lines depends entirely on identifying and managing the root cause. If an injury caused the disruption, the nail will typically grow out normally once the damage heals. In the case of systemic illnesses, managing the disease effectively will usually allow the nail matrix to return to its normal function. For nutritional deficiencies, improving diet or taking supplements can help restore healthy nail growth.
It’s worth noting that while Beau’s lines are a common nail abnormality, they are not the only one worth paying attention to. For example, spoon-shaped nails (koilonychia) can indicate iron deficiency anemia, while clubbed nails may suggest lung or heart problems. Yellow nails can point to a fungal infection or respiratory condition, and white spots on the nails are often a sign of minor trauma or zinc deficiency.
Beau’s lines can come and go without being a cause of concern but if it’s a recurring issue or you are experiencing onychomadesis, speak to your GP about what might be the cause.
Clubbing
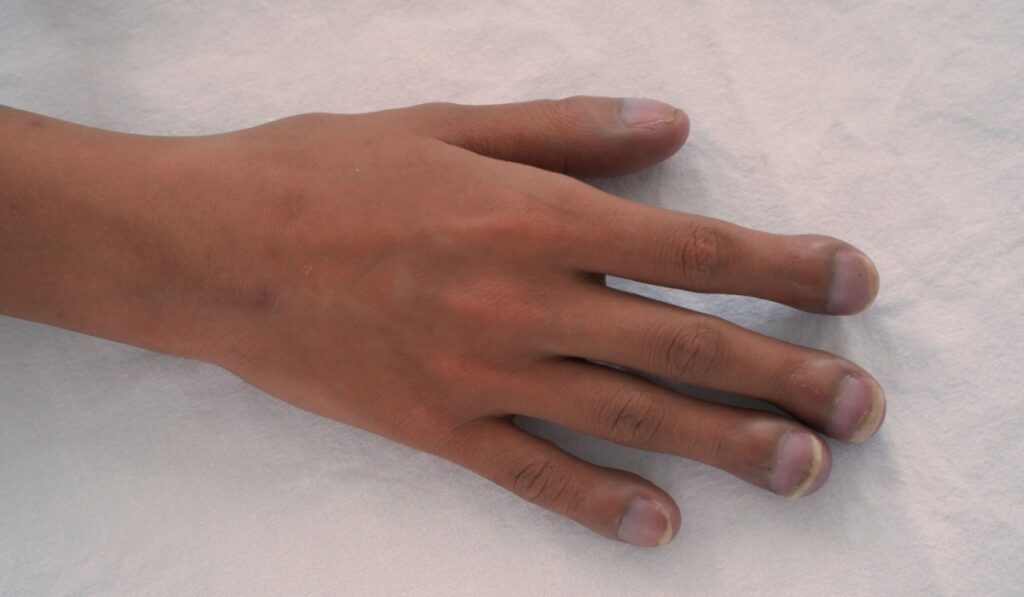
Clubbed fingernails also affect the fingertips. As the nails curve downward, the fingertips begin to swell and cause discomfort. This shift may not be noticeable since it can evolve over time. “Generally, red or purple lines under your nails are due to an injury. But if you notice these and don’t recall injuring your nail, you might want to book a doctor’s appointment because these can be a symptom of heart disease,” says Shah.
“Clubbing can also be a suggestion of heart disease, a major cause of death worldwide. This is where the nail curves over rounded fingertips or the ends of the toes, resulting in a bulbous appearance. Other symptoms that indicate heart disease include extreme fatigue, swollen ankles and pain in the chest, stomach, legs, arms, jaw or back.” Keep in mind that some people’s natural fingernails look clubbed.
Clubbing is a medical condition that can affect both your fingers and toes. It usually occurs bilaterally, meaning it impacts both hands and/or feet equally. The condition develops gradually over time and results in noticeable changes in the shape, texture, and appearance of the nails and surrounding tissues.
One of the most distinctive features of clubbing is the change in the appearance of the fingertips and nails. The nails often become red, swollen, and sponge-like, taking on a ballooned appearance. When viewed up close or from a distance, clubbed nails may resemble upside-down spoons due to their curved shape.
These physical changes usually do not occur in isolation. Clubbing is often accompanied by other symptoms, such as shortness of breath, chronic coughing, or other signs of an underlying health issue. Because clubbing is not a disease itself but rather a symptom, it is often linked to more significant health conditions, including lung diseases, heart problems, liver disease, and gastrointestinal disorders.
Features of Secondary Clubbing
Secondary clubbing refers to clubbing that develops as a result of another underlying condition. The following are key features of secondary clubbing:
- Softening of the Nails: The nails lose their firmness and become noticeably soft to the touch.
- Spongy Nail Beds: The nail beds take on a sponge-like texture when pressed.
- Floating Nails: The nails may appear to float rather than being firmly attached to the nail bed.
- Loss of the Nail-Cuticle Angle: The natural angle between the nail and the cuticle begins to disappear.
- Bulging of the Fingertips: The distal part of the fingers (where the nail meets the fingertip) may become enlarged and bulbous.
- Warm, Red Nail Beds: The nail beds often appear warmer and redder than usual.
- Downward Curving Nails: The nails curve downward, resembling the round portion of a spoon.
- Shiny Skin and Ridging: Over time, the skin surrounding the nail may become shiny, and ridges may develop on the nail surface.
Clubbing is often associated with chronic diseases, particularly those affecting the heart, lungs, liver, and gastrointestinal system.
Lung-Related Causes
- Lung Cancer: Accounting for about 90% of all clubbing cases, nearly 30% of lung cancer patients experience clubbing. It is more common in non-small cell lung cancer than in small cell lung cancer.
- Interstitial Lung Disease: This condition involves inflammation and scarring of the tissue surrounding the alveoli, the tiny air sacs in the lungs.
- Human Immunodeficiency Virus (HIV): HIV increases the risk of chronic lung diseases and infections, which may result in nail clubbing.
- Cystic Fibrosis: An inherited disease causing thick, sticky mucus to accumulate in the lungs and other organs.
- Empyema: A collection of pus in the pleural cavity, often as a complication of pneumonia.
- Bronchiectasis: Permanent scarring and widening of the airways, leading to mucus buildup and persistent coughing.
- Sarcoidosis: An inflammatory disease that can alter the structure and function of lung tissue.
- Other Lung Conditions: Idiopathic pulmonary fibrosis and pulmonary tuberculosis are also linked to clubbing.
Heart-Related Causes
- Congenital Heart Disease: Heart defects present from birth, especially cyanotic heart disease, often cause clubbing.
- Infectious Endocarditis: An infection of the inner lining of the heart chambers and valves, usually caused by bacteria.
- Aortic Aneurysm: A balloon-like bulge in the aorta, the primary artery carrying blood from the heart.
Other Systemic Causes
While clubbing is most commonly linked to heart and lung conditions, other systemic diseases can also contribute:
- Endocrine Disorders: Hyperthyroidism, particularly Graves’ disease, has been associated with clubbing.
- Celiac Disease: A chronic autoimmune disorder causing damage to the small intestine in response to gluten.
- Cirrhosis: Advanced liver disease where scar tissue replaces healthy liver cells.
- Crohn’s Disease: A chronic inflammatory bowel disease affecting the gastrointestinal tract.
- Ulcerative Colitis: An inflammatory condition causing ulcers in the lining of the large intestine.
- Other Cancers: Hodgkin’s lymphoma and mesothelioma (a rare cancer caused by asbestos exposure) can also cause clubbing.


